While some across the world are still grappling with PTSD from the global COVID-19 pandemic, a new outbreak quickly is gaining traction and bringing fear into the hearts of many.
As of now, the risk of monkeypox in the United States is believed to be very low. As the world deals with this new outbreak, the CDC is working closely with other countries that have seen clusters of monkeypox pop up, tracking potential cases, and conducting diagnostic testing.
Misinformation is running rampant, so here's everything you need to know about monkeypox.
History
Unlike COVID-19, monkeypox is a disease people have known about for decades. According to the CDC, "Monkeypox was first discovered in 1958, when two outbreaks of a pox-like disease occurred in colonies of monkeys kept for research." While the disease is referred to as "monkeypox," scientists have not confirmed that it is necessarily linked to monkeys and say it is just as likely to spread from rodents.
After its initial discovery, monkeypox still had not infected a human being. It wasn't until 1970 – nearly 12 years later – that the disease first reached a person. Since then, nearly all reported cases have been found in people who either live in or visited central or western African countries.
The current global outbreak is the largest spread of monkeypox scientists have ever seen. They believe this can be pinpointed back to a family in London who came down with the disease after a single family member traveled to Nigeria, where there is currently experiencing an outbreak.
Global cases have shown that monkeypox has now reached Spain, Portugal, Sweden, the US, and Canada. Scientists believe the spread is the result of community transmission.
What is monkeypox? How is it treated?
All the talk about "global spread" and "community transmission" has many worried that monkeypox could be the next COVID-19, but scientists reassure us that this is not the case. For starters, a vaccine is already available.
Unlike COVID-19 or the flu, monkeypox is not known to have complex, multiplying strains, which means that a single set of vaccinations is likely to prevent contracting the disease for a lifetime. Also, like with smallpox or chickenpox, exposure to the disease should allow the body to become immune to it over time.
The Department of Public Health already has a plan of attack for monkeypox. "We'd like to do what we did with smallpox to eradicate it: ring vaccination. If you see a case and then you vaccinate the people around that case, you can stop the spread of the disease. Unlike many other diseases, you can vaccinate somebody after they've been exposed, and it will stop or at least lessen the severity of the disease."
The DPH has already approved three different vaccines to prevent monkeypox. "One vaccine is licensed for monkeypox as well as smallpox and is a two-shot vaccine: one shot initially and another shot four weeks later. The other [two] are one-time vaccinations," the DPH website said.
For someone already experiencing symptoms of monkeypox, the vaccine can still be effective. "The Jynneos vaccine is effective in preventing monkeypox disease up to four days after exposure and may reduce the severity of symptoms if given up to 14 days after exposure," the Kaiser Family Foundation reported.
Are you at risk for monkeypox?
Despite growing concern over the spread of monkeypox, the CDC is still only recommending vaccination against the disease for those at heightened risk. This includes people who have come in close contact with someone who tested positive for monkeypox, men who have sex with other men, and Trans women who have had multiple sex partners in a venue where there was known to be monkeypox or in an area where monkeypox is spreading.
Currently, healthcare workers, laboratory staffers, first responders, and certain members of the military are most likely to be exposed.
While the CDC reports that monkeypox has spread most quickly among men who have sex with men, doctors believe these numbers are likely because LGBTQ+ people are more attuned to watch out for signs of STD, like syphilis, which monkeypox often mirrors.
"It could also be that because monkeypox can look initially like the rash from syphilis, people who are particularly attuned to and watching for signs of syphilis would seek medical attention sooner than other people," read a report by the CDC.
Monkeypox is also not a disease that strictly links to Gay men. As of June 27, the European Centre for Disease Prevention and Control reported 10 cases among women.
While transmission of monkeypox requires much more intimate contact than the transmission of a disease like COVID-19, it is not an STD. This is because it can be spread through nonsexual acts of intimacy. "If someone were coughing in your face, spit or drooled on you, probably also kissing – it spreads through those kinds of contacts, rather than just being in a room with somebody. But it does also persist on clothing and bed linens, for example," according to the Johns Hopkins Institute of Public Health.
No accounts of monkeypox spreading through aerosols, like COVID-19 does, have been documented so far. The CDC says that asymptomatic people cannot spread monkeypox.
The CDC is now warning against going to raves or other parties where people come in close contact with each other and wear little clothing. This also includes saunas and sex clubs. It also recommends always washing sex toys and bedding after intercourse.
It also notes that condoms and dental dams can help reduce the risk of contracting monkeypox but do not prevent all transmission, because they only protect the surfaces of the skin that are covered by them. The monkeypox virus can enter broken skin and penetrate mucous membranes or open orifices (such as the eyes, nose, mouth, genitalia, and anus).
Symptoms
Monkeypox is considered a mild disease and has a less than 1% mortality rate. All who have died of the disease have been people living in developing nations who lack access to advanced medical care.
Scientists do warn, however, that despite monkeypox being mild, it can still become serious, or even deadly, for immunocompromised people, pregnant people, newborns, young children, and those with skin conditions such as eczema.
Monkeypox has been described as a milder version of smallpox. Symptoms typically develop within 21 days of exposure and can include fever, chills, swollen lymph nodes, rash, and headaches.
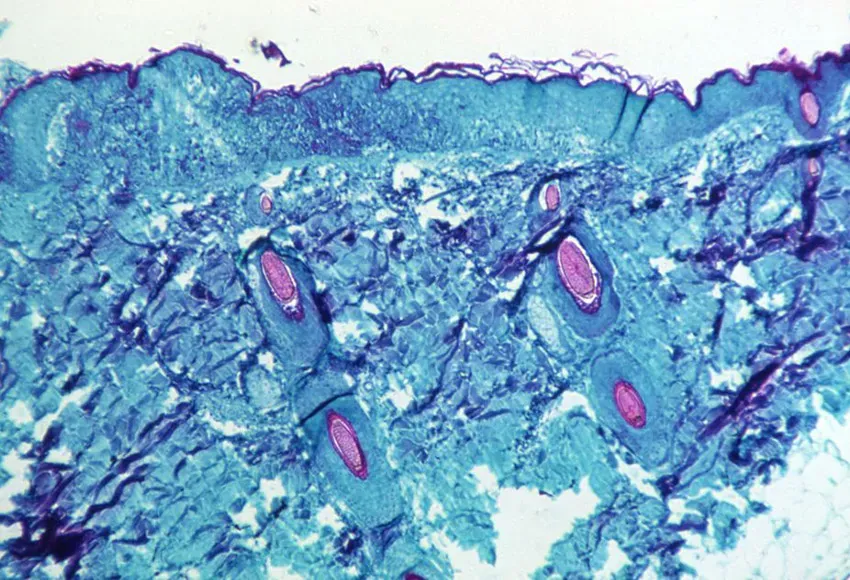
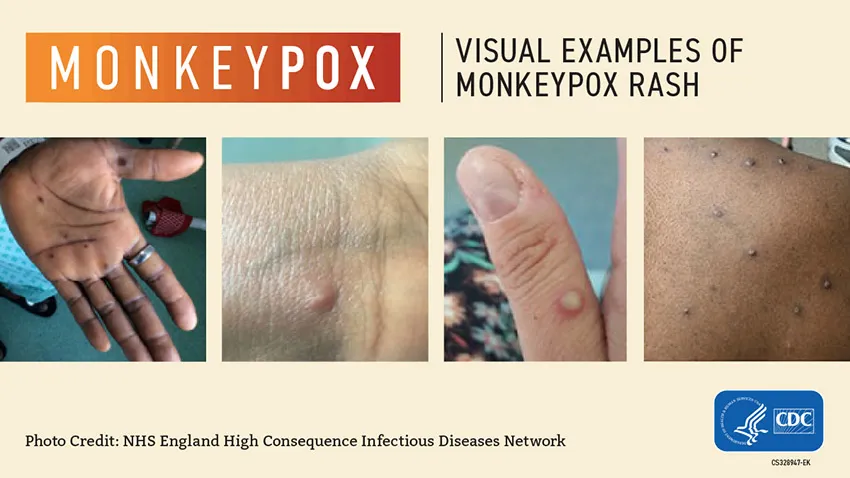
The most notable symptom of monkeypox is the rash, which will start with red spots that eventually develop into pus-filled bumps that can resemble pimples or blisters. Those who have experienced monkeypox describe the rash as painful.
Typical outbreaks in West Africa often see the pox appear on the palms of hands and soles of feet, but the new global outbreak has reported more lesions around the genitalia and mouth – similar to herpes.
The pox eventually opens into sores and then scabs over. People with monkeypox are considered most infectious when the sores open up and remain infectious until they scab over and fall off.
Healthcare professionals warn that anyone who believes they have symptoms of monkeypox, including oral, genital, or anal lesions, should go to their nearest sexual health clinic for testing. Unlike with COVID-19, a person who tests positive for monkeypox does not need to isolate away from others in their own home. As the disease is usually spread through close and intimate contact, washing hands, bedding, and clothes, and keeping one's distance from others in public places should be enough to help stop the spread.
Monkeypox is considered a zoonotic disease, which means, like COVID-19, there is a chance it can spread to wild and domestic animals that come in contact with it. However, the CDC does not believe this strain to be a risk to pets, though it still recommends avoiding contact with pets if you test positive for monkeypox until symptoms subside.
The world has changed tremendously since 2020, and how we handle and approach global disease outbreaks has shifted before our eyes. While monkeypox does not pose a severe threat in the same way COVID-19 has, doctors, scientists, and everyday people are approaching the situation with hypervigilance to prevent another global catastrophe.