Michael first knew something was off in the shower.
Overnight, he had developed an embarrassing rash. It didn't hurt much at first, but by the end of the day, that changed.
"It was really a zero-to-sixty kind of emergence of those sores," Michael (not his real name) told the SGN. "I immediately knew something was wrong."
He knew right away that this was the first symptom of mpox, having been exposed before the symptom appeared.
Mpox has impacted Michael's life in every way imaginable. Now, in home-based isolation, his social, romantic, and family lives have all been on hold. "If I didn't work remotely, I know that it would affect my job life," he said. "You'd have to disclose to your employer, and that would be an awkward thing."
Facts about mpox
Mpox, formerly called monkeypox, caused by a highly contagious virus, first broke out in the US in May of 2022, affecting mostly sexually active Queer men. Once rare, it has since become a significant public health concern.
Mpox features clusters of painful, blistering sores and skin rash, usually on the genitals or anus. It can affect anywhere that has come into contact with an active infection. The blisters and rash produce a burning, needle-like sensation that can cause moderate to severe pain and interfere with daily functions, like bathroom use. Mpox sometimes also comes with flu-like symptoms and swollen lymph nodes.
The illness is rarely fatal, but deaths do occur – especially among children, older adults, and those with serious long-term health issues.
Mpox has an incubation period of about 1-3 weeks and sometimes longer before the start of symptoms, which usually last for 2-4 weeks, or longer for those with compromised immune systems.
Mpox is spread by close, skin-to-skin contact, which does not have to be sexual. It is not prevented by barrier methods of safer sex protection such as condoms, but there is a vaccine available.
A resurgence of cases
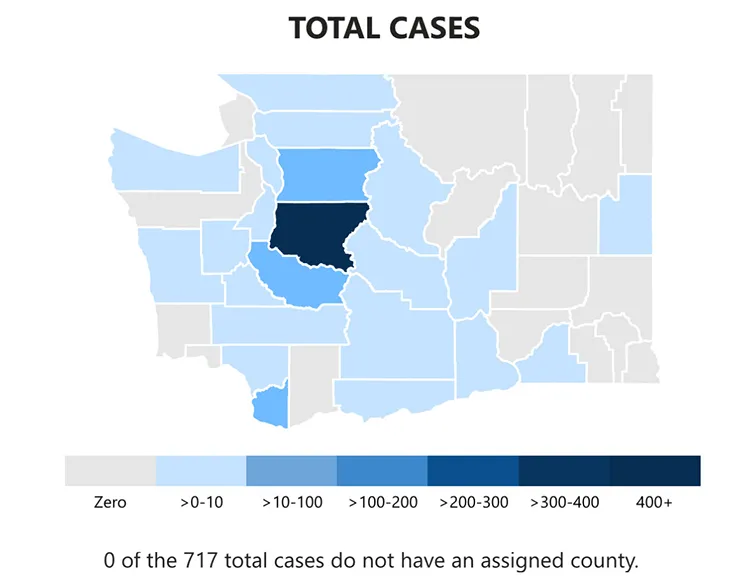
Michael may be in isolation, but he is not alone. According to the tracking data on the Washington State Department of Health's website, mpox infections in the state are up to 717 active cases as of November 6, an over 700% increase since the beginning of September. Those include 21 hospitalizations and, thankfully so far, zero deaths. Of these new infections, 76.6% of them are located in King County.
In an email to the SGN, Mark Johnson, a public information officer with the WSDOH, explained that "new cases could be increasing for a variety of reasons," noting that the current outbreak seems chiefly to affect men who have sex with men and their sexual networks.
Health officials in California and Oregon have already issued alerts, though no health department in Washington is yet to raise an alarm.
On why these infection rates are rising, Johnson said that public health and community members are still trying to understand the problem, but he pointed to large, nationally known events such as Folsom Street Fair, Southern Decadence, and Mates Leather weekend, as well as private sex parties here in Washington.
Importantly, Johnson lauded the way Queer communities have taken care of each other, explaining that "people that have hosted parties have done a great job at notifying guests about possible exposures and providing resources on where people can get tested and vaccinated."
Johnson wants to remind people that mpox is not a "Gay" virus. "While this has been disproportionately affecting people in the Gay male and Queer communities, we must stress that mpox does not exclusively affect members of this community," he said.
Crucially, "If someone notices any new symptoms that may be mpox, even after receiving one or two doses of vaccine, folks are encouraged to see a medical provider," Johnson added.
Seeking treatment
Michael met a number of challenges when seeking healthcare and treatment.
"I had a very mixed experience with my medical provider," he said. While his family care doctor got him in right away – giving him an exam, sending off labs, and doing basic STI tests – they didn't give him much reassurance. His provider knew very little about mpox, as they are not focused on Queer male sexual health.
His provider didn't know how or where to obtain antiviral drugs, and it took a staggering ten days for his lab results to come back.
"I was kind of left out to dry a little bit there," he said. "My symptoms were getting pretty bad pretty quickly. ... I feel like I was given some inaccurate information by my primary care doctors, which felt pretty bad, and my labs took way longer than they should have, which stymied me getting early treatment."
Eventually he contacted Harborview Sexual Health Clinic through the University of Washington, which provided him the experimental drug tecovirimat (Tpoxx) through an emergency-use authorization – meaning he wouldn't have to undergo experimental trial protocols or risk receiving a placebo. Once he was on it, his symptoms improved dramatically within only 1-2 days.

Preventing mpox
Mpox is largely preventable through a two-dose course of vaccinations taken one month apart. The vaccine, called JYNNEOS, is available at most public health departments, medical providers, and sexual health clinics, including Harborview.
Johnson said that the efforts to roll out the vaccine during the outbreak in 2022 likely helped prevent this resurgence from being worse so far.
He cautioned, though, that "while the mpox vaccine is highly effective, it may not always prevent infection. It can, however, reduce painful symptoms and hospital visits relating to mpox," and that getting the vaccine is worth the time it takes to find it.
Michael reported that he and all the people in his chain of infection are vaccinated, and that he's grateful the infection wasn't more severe.
Nonetheless, he and public health officials have the same message to anyone at risk of mpox and its impact on their lives: in the words of Johnson, "The mpox outbreak is not over. Please get vaccinated, get tested, talk to those around you about mpox and sexual health, and stay safe!"
For more information about mpox, including facts about transmission, symptoms, vaccines, and treatment, visit the Centers for Disease Control's website at https://www.cdc.gov/poxvirus/mpox
To find vaccines and treatment here in King County, contact Harborview Sexual Health Clinic at 206-744-3590.